With cervical cancer ranking as the second most common cancer among women in Sri Lanka, urgent action is necessary to address the pressing public health concern.The Ministry of Health spearheads initiatives to eliminate cervical cancer across the country.A pilot project carried out in Kalutara demonstrates encouraging results with HPV DNA testing in early detection and lowering cervical cancer rate in Sri Lanka.
Cervical cancer ranks as the second most common cancer among women in Sri Lanka, accounting for an estimated 1,407 diagnoses and 780 deaths each year.1 Without intervention, projections forecast a potential death toll of 58,754 by 2070 and 115,137 by 2120.2
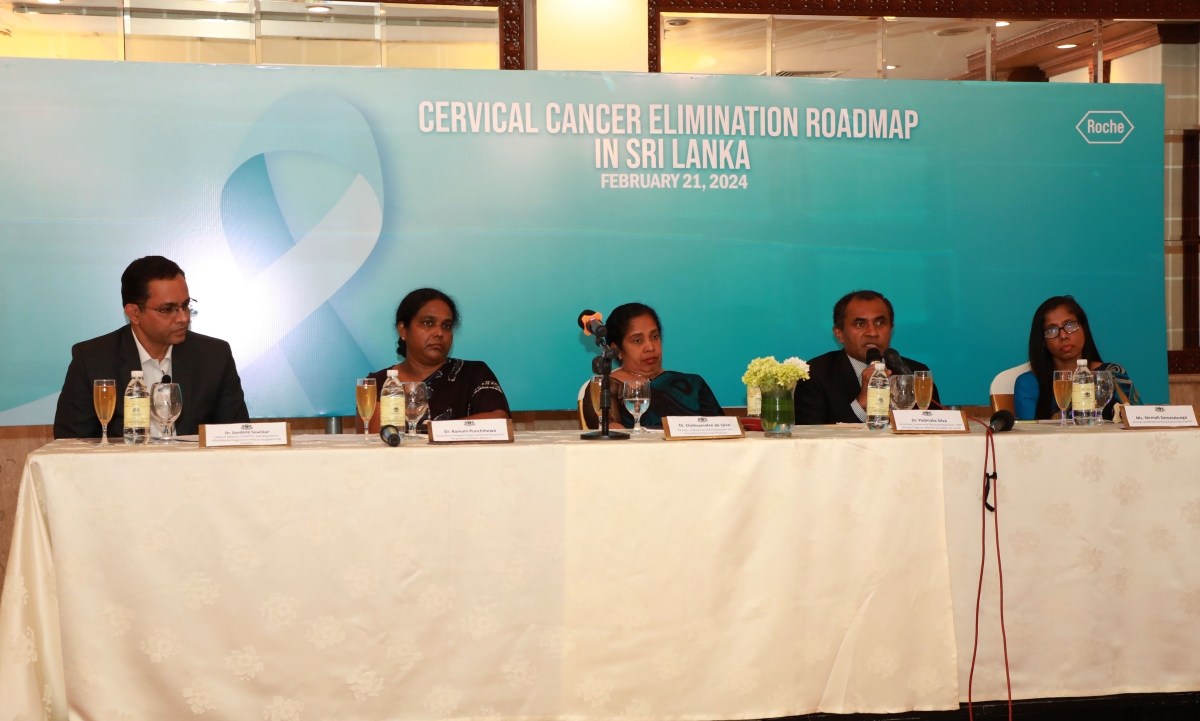
Addressing this urgent need to eliminate cervical cancer elimination, a panel discussion was convened comprising experts such as Dr. Chithramalee de Silva, Director of Maternal and Child Health and Consultant Community Physician; Dr. Ramani Punchihewa, Consultant Histopathologist at the National Hospital for Respiratory Disease; Dr. J Padmaka Silva, Consultant Community Physician and National Program Manager for the Well Woman Program; and Nirmali Samaratunga, Chairperson, Rotary Cervical Cancer Elimination project. Moderated by Dr. Sandeep Sewlikar, Head of Medical, Scientific, and Regulatory Affairs at Roche Diagnostics India & Neighbouring Markets, the discussion highlighted the steps taken by Government of Sri Lanka towards the elimination of the cervical cancer, programs undertaken like Well Women Clinic, pilot project in Kalutara district to analyse different methods of cervical cancer screening among ever-married women in 35-year and 45-year cohorts, and steps taken by the Family Health Bureau to align cervical cancer elimination targets with that of World Health Organisation’s (WHO) goals.
Key highlights of the Kalutara project:
- A comparative analysis assessed the effectiveness of various screening methodologies such as Pap smear, LBC and HPV DNA to determine the most effective screening method for detecting indications of cervical cancer among married women aged 35 to 45.3
- The findings showcased that the Cervical Intraepithelial Neoplasia (CIN) detection rate by colposcopy was higher with HPV DNA screening than other methods.3
The panellists also discussed the WHO recommendation of using HPV-DNA based detection as the primary screening method, starting at the age of 30 years, with regular testing every 5–10 years.3 A thorough examination of the current cervical cancer screening landscape in Sri Lanka was presented, along with detailed plans for expanding screening programs to reach a broader demographic. Furthermore, Nirmali Samaratunga illuminated the crucial role played by organisations such as the Rotary Club of Colombo in raising awareness and facilitating access to cervical cancer screening programs across the country.
Dr. Chithramalee said, “Proactive initiatives like policy advocacy, health system strengthening, increasing coverage & equity, quality of care, and raising community awareness on screening are being undertaken by the Well Women Program, Ministry of Health, Sri Lanka. Based on the evidence that has been generated worldwide on the effectiveness of different screening methods used by many countries for cervical cancer screening, HPV DNA testing has been identified as the most effective. Hence, the government of Sri Lanka has taken a decision to introduce HPV DNA based screening in phase wise manner.
Dr. Padmaka Silva added, “Through vaccination, early screening, and education, we aim to make significant strides towards eliminating cervical cancer. To screen 70% of women with high precision tests we have introduced HPV DNA as the primary screening test for cervical cancer from 2020 onwards. With our extensive network of 1000 Well women clinics in 354 public health units in nine provinces in the country, we have made significant strides for cervical cancer screening and hope to expand the screening program in a phased manner with HPV DNA in all districts in the country by 2030.”
Dr. Sandeep Sewlikar concluded with the crucial need for a multipronged strategy to tackle cervical cancer in Sri Lanka. He expressed his gratitude to the dedicated team involved in executing the project, while also recognising their commitment and hard work as pivotal in advancing the fight against cervical cancer in the country. “We are inspired by Sri Lanka's efforts and are delighted to support the Family Health Bureau, Ministry of Health, Sri Lanka as a diagnostics provider. With the WHO prequalification for our cobas HPV test, we are confident that together we can help countries overcome this preventable cancer and empower women through timely screening.”